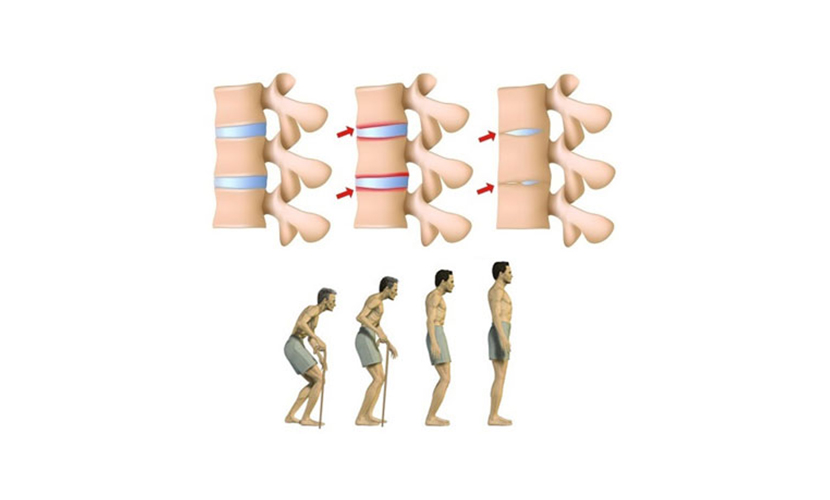
Ankylosing Spondylitis is a type of arthritis that affects the spine. Symptoms include pain and stiffness that extends from the neck to the lower back. Spinal bones (vertebrae) can grow or fuse to cause stiffening. These changes can be moderate or advanced and may lead to hunchback. Early diagnosis and treatment can prevent pain and stiffness and prevent deformations.
Who is affected by Ankylosing Spondylitis?
It affects 0.1% -0.5% of the adult population. Although it can occur at any age, it mostly catches men at puberty or in their 20s. It is less common in women, or is softer; mostly seen in some Native Americans.
What are the symptoms of ankylosing spondylitis?
Among its early symptoms:
Pain and stiffness: Continuous pain in the lower back, gross meats and hips, lasting more than 3 months. Usually, spondylitis usually begins around the sacroiliac joint around the lower posterior part of the pelvis, where the sacrum joins the ilium bone.
Bone union: Bony fusion. Ankylosing spondylitis can cause the bones to grow too much and bone fusion. This fusion, which affects the neck, back and hips, may prevent the person from performing daily activities. Boiling the ribs into the spine or chest bones can prevent a person from breathing deeply and expanding their chest.
Pain in ligaments and tendons: Pain in ligaments and tendons.Spondilites can affect some ligaments and tendons that attach to bones. Tendonitis (inflammation of the tendons) can cause stiffness in the back of the ankle or in the Achilles tendons behind the ankle.
Ankylosing spondylitis is a systemic disorder, that is, its symptoms may not be limited to joints. These patients may also have complaints such as fever, fatigue and loss of appetite. Eye inflammation (redness and pain) can also be seen. In less common cases, liver and heart conditions may develop.
What causes ankylosing spondylitis?
Although the cause of ankylosing spondylitis is unknown, there is a close link with hereditary. Most patients with ankylosing spondylitis have a gene called HLA-B27, if not all. People with this gene are prone to spondylitis, but in 10% of them, the disease may not occur.
How Is Ankylosing Spondylitis Diagnosed?
Many factors play a role in the diagnosis of ankylosing spondylitis:
begin to show symptoms on
Results of the physical test
Pelvis and back x-rays
Chest measurements while breathing
Laboratory results
How Is It Treated?
Ankylosing spondylitis has no cure, but treatments reduce discomfort and increase movement. The goal of treatment is to reduce pain and stiffness, have a good posture, prevent deformation and enable normal activities. When properly treated, patients with spondylitis can continue their normal lives. Under normal circumstances, the spondylite teamwork approach is recommended. The team consists of the patient, doctor, physiotherapist and occupational therapist. In many deformed patients, osteomoty and fusion can be performed.
Physical and occupational therapy Physical and occupational therapy: Physical and occupational therapy and early intervention are important to maintain function and minimize deformation.
Exercise: Daily exercise program will work to reduce stiffness, strengthen the muscles around the joints and minimize the risk of disability. Deep breathing exercises will help maintain the flexibility of the rib cage. Swimming is a great exercise for these patients.
Medication: Some medications reduce pain and stiffness, and patients are allowed to do the exercises with minimal discomfort. Non-stereoid anti-inflammatory drugs (NSAIDs) - drugs such as ibuprofen, naproxen, and aspirin are among the most commonly used drugs. In mild cases, drugs can be added to the treatment regimen. Anti-arthritic drugs, methotrexate, NSAIDs that modify the disease can be used in cases where it is insufficient to reduce pain. In addition, new medicines called biological, Cimzia (certolizumab pegol), Enbrel (etanercept), Humira (adalimumab), Remicade (infliximab) and Simponi (golimumab) are approved by the FDA. Anti-depressant Cymbalta is also approved for chronic pain. In some cases, it may also be helpful to inject steroids into joints or tendons.
Surgery: In some advanced patients, if the knees or hip are affected, an artificial joint can be a treatment element.